Bladder management
What is the relationship between the spinal cord and the bladder?
A spinal cord injury (SCI) will always affect the control you have over your bladder at any stage. During post-injury rehabilitation, you will learn techniques to empty your bladder. These strategies will be tailored to your individual needs and will take into account your activity and skill level.
It is important to understand how your body works
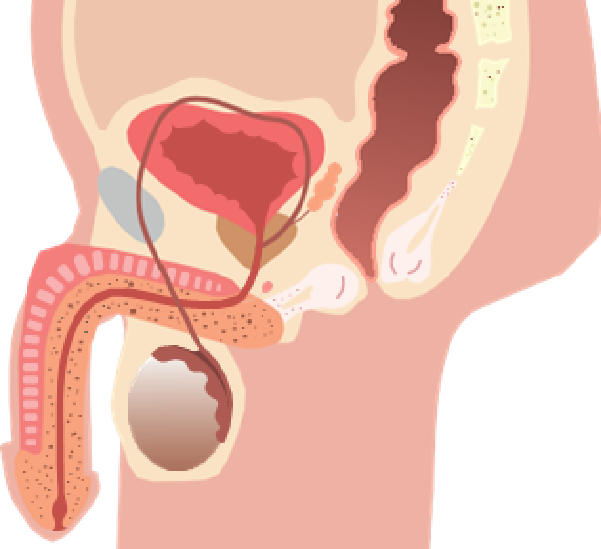
The urinary system consists of the kidneys, two ureters, the bladder, and the urethra.
Kidneys work 24/7 to remove waste from your body through your bloodstream. This waste becomes urine. Urine is a mixture of excess salts and water that exits the kidneys through the ureters, one from each kidney into the bladder. The ureters allow urine to flow in one direction and are connected to the bladder

How does the bladder work?
The bladder is a muscular sac that stores urine until it is convenient to empty it. Once the bladder is full, nerves send a message to the brain via the spinal cord.
When you decide to urinate, the brain sends messages through the spinal cord to the bladder wall muscles, telling them to contract. The sphincter opens, and the bladder releases urine, which passes through the penis or genitals into the urethra.
Urine is usually straw coloured but seek medical advice if there is an unusual smell, colour or change in blood. Certain foods and medications can affect the colour and smell of urine.
How does the bladder work after an injury?
Damage to the spinal cord also damages your body's bladder control system. Nerves no longer communicate with the brain and therefore cannot transmit messages. The bladder fills as before, but the awareness of fullness and the ability to control the flow of urine are altered.
A lesion at the T12 level or above is called a reflex bladder, also known as an automatic or spastic bladder. Injuries below T12 can cause a flaccid, or flaccid, bladder. It is possible to have elements of both.
What is reflex bladder?
A reflex bladder is where the neural pathway and nerve impulses between the bladder and spinal cord – known as the reflex arc – remain intact but messages no longer reach the brain. A reflex bladder allows automatic, involuntary control of the bladder, meaning that when the bladder fills above a certain level, it contracts, and urine flows out automatically.
However, a reflex bladder may not empty completely due to the sphincter not relaxing fully. This can leave a pool of urine in the bladder, known as residual urine, which increases the risk of infection. The pressure from bladder contractions can cause back pressure on the kidneys.
What is an areflexic bladder?
An areflexic bladder is where the reflex arc between the bladder and spinal cord is damaged. The impulses to the spinal cord are interrupted, so the bladder does not receive the message that it needs to empty.
An areflexic bladder has no muscle tone and, therefore, does not contract automatically to allow it to empty. It continues to fill, and small amounts of urine may leak out. The areflexic bladder needs emptying at regular intervals, and this can be achieved by intermittent self-catheterisation.
What is an areflexic bladder?
An areflexic bladder is where the reflex arc between the bladder and spinal cord is damaged. The impulses to the spinal cord are interrupted, so the bladder does not receive the message that it needs to empty.
An areflexic bladder has no muscle tone and, therefore, does not contract automatically to allow it to empty. It continues to fill, and small amounts of urine may leak out. The areflexic bladder needs emptying at regular intervals, and this can be achieved by intermittent self-catheterisation.
What is bladder management?
Bladder management is a personal programme developed during rehabilitation that allows you to gain as much control over your bladder as possible.
The main aims of bladder management are to:
- Establish a safe method for emptying your bladder at intervals throughout the day to protect your kidneys and help you stay dry
- Establish a long-term routine to help you achieve independence, improve your quality of life, allow you to carry out daily activities and enjoy a social life
- Maintain a good body image
- Reduce the risk of complications, such as bladder and kidney infections and the formation of bladder stones
- Correct bladder management is vital to your health and wellbeing. Urinary tract complications are still among the leading causes of illness, readmission to hospital and death in SCI people
What are my bladder management options?
In the first few weeks after SCI, the bladder will need to be emptied regularly through a catheter, a fine, flexible tube that carries urine out of your bladder.
During rehabilitation, you will be educated on the best method for emptying your bladder. This will depend on:
- The level of injury
- Whether your bladder is reflex or areflexic
- Whether you are male or female
- What is acceptable to you
- Results of urological investigations
- What is least likely to cause major complications, such as bladder stone formation, infection and autonomic dysreflexia (AD)
Catheters
There are three main types of catheters:
1. Indwelling urethral catheters
These are inserted through the urethra and held in place by a small water-filled balloon. This is typically a short-term solution for emptying the bladder, for example, before and after surgery or when you are away from home if you cannot rely on access to toilets to self-catheterise.
Things to be aware of with indwelling urethral catheters
- They can be convenient, but long-term use is best avoided as it can cause urethral dilation, chronic bladder infection, penis splitting and bladder stones.
- They can be easily blocked by sediment and small calcium granules that gather around the balloon and grow to form stones
- May require regular bladder washouts (care must be taken during this procedure)
- Need to be changed regularly, every four to six weeks
- Often need to be inserted by a PA or district nurse
- Require extra care to ensure good sterile technique
- Require you to increase your daily intake of fluid to 3.5 litres (6 pints)
- Can increase the risk of infection as bacteria can enter through the catheter’s permanent opening
- Can sometimes be expelled by spasms or because of a blockage or stone
- Require securing to the thigh to prevent urethral trauma
- Can cause leakage around the catheter during menstruation
2. Intermittent catheters (self-catheterisation)
This method is used for draining the bladder without a permanently fitted catheter. The catheter is inserted into the bladder every few hours to drain it.
Intermittent catheters are often the method of choice for people with an areflexic bladder, and they are commonly used by those with paraplegia. If you have a reflex bladder with good capacity, you can also use this method. Medications might be needed to increase bladder capacity.
People with some hand control can learn to self- catheterise, but you need to be sufficiently dexterous to avoid the risk of damaging the urethra. Your chance of infection is significantly reduced if you change your own catheter than if someone else changes it for you.
Both men and women can usually self-catheterise while in bed, in a wheelchair or on the toilet.
Remember that you will need privacy and access to a toilet, which can sometimes be difficult if you are away from home.
It’s essential to use good technique and hygiene practices when self-catheterising. Avoid bladder infections wherever possible, and ensure you wash your hands and genital area thoroughly before passing the catheter.
Benefits of intermittent self-catheterisation include:
- The ability to empty your bladder completely at regular intervals
- Achieving continence without the need to wear an appliance
3. Suprapubic catheters
A suprapubic catheter is an indwelling catheter inserted into the bladder via a small surgical incision made in the abdomen below the belly button.
Would a suprapubic catheter be suitable for me? These are typically used by:
- Newly injured people
- Tetraplegic women
- People who do not have the manual dexterity to carry out intermittent self-catheterisation
A suprapubic catheter is inserted through a hole in your abdomen into your bladder. The incision is not permanent and starts to close within 24 hours if the catheter is permanently removed.
The catheter used is similar to that used for urethral use. The insertion of it may initially cause an increase in spasms. People with suprapubic catheters may experience oozing around the catheter site, and this should be cleaned each day as part of a regular bathing routine. A dry gauze dressing may be applied each day.
Suprapubic catheters:
- Should be changed every four to six weeks to prevent blockages
- Should be taped to the lower abdomen and connected to a leg bag
- Protect and free the genital area for sexual function
- Carry less risk of tubing being sat on or kinked
- Carry a similar risk of infection, blockage and stone formation as an indwelling urethral catheter
If the catheter becomes blocked, urine may drain via the urethra, and you may not realise you are sitting in wet clothing. Bladder washouts will help remove any build-up of deposits that may form bladder stones. It is essential to drink plenty to keep the urine as diluted as possible.
The Urinary System
Sheaths and condoms
This form of bladder management can be used by men with reflex bladders. A urinary sheath or condom is applied to the penis and attached by a plastic tube to a collecting bag strapped to the leg or abdomen or hung beside a bed.
Many varieties are available in assorted widths and lengths to ensure the best fit. Also available are latex and non-latex hypoallergenic sheaths to reduce skin problems.
Urinary sheaths are purpose made. They have a tube outlet at the end, designed to resist twisting or tearing, and usually come with an adhesive coating on the inside of the sheath.
Inspect your penis carefully and stop using a sheath or condom immediately if there are signs of a rash, red marks or broken skin. If the area becomes particularly sore, an indwelling urethral catheter can be used for a brief period to allow the skin to heal.
What other equipment is available for bladder management?
Catheter valve
A catheter valve is a tap-like device designed to fit into the end of a urethral or suprapubic catheter.
The valve can be switched on or off to drain urine from your bladder or stop drainage. You can close the valve for up to four hours at a time to ensure your bladder fills regularly. It’s worth noting that if the bladder is regularly left empty, it could reduce the amount of urine your bladder can hold.
Drainage bags
Urine drainage bags are connected to a sheath, condom or catheter by plastic tubing. Different bags can be worn on the upper or lower leg, across the stomach, or hung beside a bed or wheelchair. They can be disposable or reusable. Leg bags, with capacities from 350ml to 1,300ml, can be attached by straps or a stocking-type sleeve. Overnight bags have larger capacities of up to 2l. These can be useful when on a long-haul flight.
Never lift a drainage bag above the bladder level unless you’re confident your system has a well-functioning non-return valve. If you are susceptible to autonomic dysreflexia, care should be taken when using a catheter valve.
What is autonomic dysreflexia?
Autonomic dysreflexia (AD) is a condition where there is a sudden and potentially lethal rise in blood pressure. It is the body’s way of responding to a problem and is often triggered by acute pain or another harmful stimulus in the body, such as an overfull bladder. The condition is unique to SCI people and most commonly affects those with injuries at or above T6 level. The rapid rise in blood pressure (hypertension) can lead to a stroke (cerebral haemorrhage) and even death. If you have an injury above T6, you must understand how to prevent and manage AD. The condition should always be treated as a medical emergency.
What common bladder management problems or complications should I be aware of?
Be aware of the following signs of infection:
- Concentrated, strong-smelling urine
- Feeling unwell with flu-like symptoms
- Autonomic response (sweating, goosebumps)
- Bypassing (urine leaking around the outside of the catheter)
- Increased spasm
- Pyrexia (raised temperature)
- Pain in the lower abdomen for people with sensation
- Blood in urine
- Swollen testicles
- Persistent rash in the groin area
How should I treat a urinary tract infection?
- Increase fluid intake to try to flush out bacteria
- Ensure your bladder is emptied frequently and completely
- Try to keep your urine acidic, (cranberry capsules and vitamin C help with this)
- If you are ill or the signs of infection persist, contact your GP. A urinary tract infection (UTI) is defined as a positive urine culture indicating the growth of bacteria. Flu-like symptoms, including feeling unwell and a raised temperature, are also common
- Infection in the bladder can pass up to the kidneys and cause damage. Frequent infections can cause scarring of the bladder, affecting its ability to contract properly
Stones
- It is not unusual for stones or calculi to develop in the kidneys and bladder. SCI people are more susceptible to this because of reduced mobility, the loss of calcium from the bones of paralysed limbs (although this is typically limited to the first few months after injury) and less efficient bladder function. Smaller stones can be passed out through the bladder and urethra without being noticed
- Larger stones, however, can create an obstruction in the kidneys or obstruct an indwelling catheter, increasing the likelihood of urinary tract infections (UTI)
- The symptoms are similar to those of a UTI, with greater difficulty in passing urine and an increased likelihood of pink-tinged urine (showing the presence of blood). Hospital treatment is needed at this stage. Stones can often be broken up by ultrasound (lithotripsy) without the need for surgery or be removed through an endoscope
Reduce the risk of stone formation by:
- Increasing your fluid intake
- Cutting down on high-calcium foods, especially milk and cheese