Skin maintenance
What is a pressure sour?
A pressure sore, also known as a pressure ulcer or bedsore, is a localized injury to the skin and/or underlying tissue typically over a bony prominence, caused by pressure, shear, or friction. These injuries are common in individuals with spinal cord injury (SCI) due to factors such as decreased sensation, limited mobility, and prolonged periods of sitting or lying down.
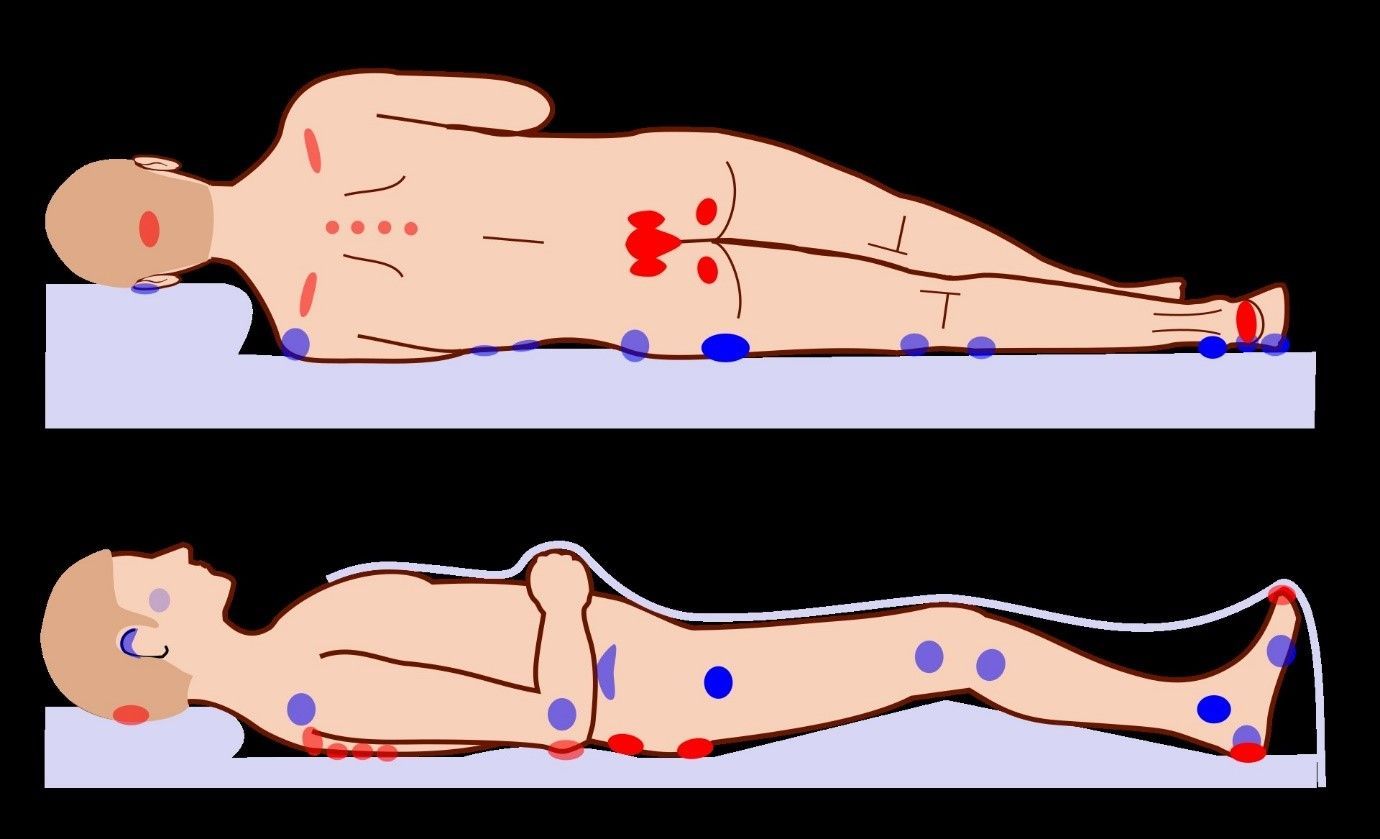
In SCI, pressure sores often occur in areas of the body where bones are close to the skin surface and are subjected to constant pressure, such as the sacrum, coccyx, heels, hips, and elbows. When pressure is applied to these areas for an extended period, blood flow to the skin and underlying tissues can be compromised, leading to tissue damage and the formation of pressure sores.
The severity of pressure sores can vary, ranging from mild skin redness (Stage 1) to extensive tissue damage involving muscle and bone (Stage 4). Without proper prevention and management, pressure sores can lead to serious complications, including infection, tissue necrosis, and even systemic illness.
Preventing pressure sores in individuals with SCI involves strategies such as regular skin inspections, pressure relief techniques, proper positioning, skin hygiene, nutrition, and hydration. It's crucial for individuals with SCI and their caregivers to be vigilant in preventing pressure sores and to seek prompt medical attention if any signs of skin breakdown are detected.
Overall, pressure sores are a significant concern in individuals with SCI, but with proper prevention and management, their occurrence can be minimized, and their impact on health and quality of life can be reduced.
What are the levels and treatment of pressure sour
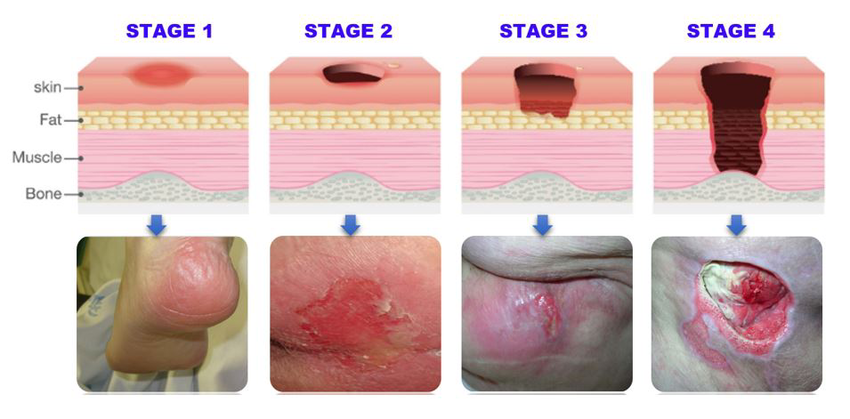
Pressure sores, also known as pressure ulcers, can be categorized into different stages based on their severity. The staging system commonly used is provided by the National Pressure Injury Advisory Panel (NPIAP). Here are the stages along with their corresponding descriptions and treatment approaches, particularly in the context of spinal cord injury (SCI):
1.Stage 1 :
• Description : In this stage, the skin is intact but shows persistent redness that does not fade when pressure is relieved. This indicates potential damage to deeper tissues.
Treatment :
• Relieve pressure on the affected area by changing positions frequently.
• Use pressure-relieving cushions or mattresses to reduce pressure.
• Keep the skin clean and dry.
• Apply moisture-barrier creams to protect the skin.
2.Stage 2 :
• Description : Stage 2 pressure ulcers involve partial-thickness skin loss, typically presenting as an open sore or blister. The underlying tissue may be visible.
Treatment :
• Clean the wound with a gentle saline solution.
• Apply dressings appropriate for partial-thickness wounds, such as hydrocolloid or foam dressings.
• Protect the wound from further trauma and pressure.
• Monitor for signs of infection, such as increased redness, warmth, or drainage.
3.Stage 3 :
• Description : Stage 3 ulcers involve full-thickness skin loss with damage to underlying tissue layers, such as fat, but not extending through the fascia.
Treatment :
• Debridement of necrotic tissue may be necessary to promote wound healing.
• Use appropriate dressings to maintain a moist wound environment and promote granulation tissue formation.
• Manage infection with antibiotics if present.
• Consider advanced wound therapies such as negative pressure wound therapy (NPWT) or bioengineered skin substitutes.
4.Stage 4 :
• Description : Stage 4 pressure ulcers are the most severe, involving full- thickness skin loss and extensive tissue damage, including muscle, bone, or supporting structures (tendons, ligaments).
Treatment :
• Surgical intervention may be required to remove necrotic tissue and repair underlying structures.
• Wound management techniques such as NPWT or specialized dressings may be utilized.
• Aggressive infection management is essential to prevent systemic complications.
5.Unstageable Pressure Ulcers :
• Description : Some pressure ulcers are covered by eschar (thick, black, necrotic tissue) or slough (yellow, fibrous tissue), making it difficult to determine the extent of tissue damage.
Treatment :
• Debridement to remove necrotic tissue and expose the wound bed may be necessary.
• Once the extent of tissue damage is visible, appropriate wound management strategies can be implemented based on the ulcer's stage.
For individuals with SCI, preventing pressure ulcers is paramount, given the increased risk associated with decreased mobility and sensation. Regular skin assessments, meticulous skin care, pressure redistribution techniques, and early intervention are essential components of pressure sore management. It's crucial for individuals with SCI to work closely with healthcare providers, including wound care specialists and rehabilitation professionals, to develop and implement a comprehensive plan tailored to their specific needs.
How to avoid pressure sour
Pressure sores, also known as pressure ulcers or bedsores, are a significant concern for individuals with spinal cord injury (SCI) due to reduced sensation, impaired mobility, and prolonged periods of immobility. Pressure sores develop when prolonged pressure on the skin restricts blood flow to underlying tissues, leading to tissue damage and, in severe cases, ulceration. Here are some strategies for preventing and managing pressure sores in individuals with SCI:
1. Frequent Position Changes for pressure relief:
Implement a schedule for pressure relief, especially for individuals who use wheelchairs or spend prolonged periods in bed. Change positions frequently to relieve pressure on vulnerable areas. Consider using pressure-relieving cushions, mattresses, or pads.
2. Proper Seating and Positioning: Ensure that individuals using wheelchairs have proper seating that fits well and provides adequate support. Use cushions or padding to distribute pressure evenly and minimize friction.
3. Weight Shifts and Transfers: Encourage frequent weight shifts and transfers for individuals with SCI who are seated for extended periods. Teach proper techniques for weight shifts and transfers to minimize pressure on bony prominences.
4. Avoiding Shear and Friction: Minimize shear and friction forces on the skin by using proper lifting and transferring techniques. Ensure that clothing and bedding are smooth and free from wrinkles.
5. Pressure-Relieving Equipment: Specialized cushions, mattresses, and padding can help distribute pressure more evenly and reduce the risk of pressure sores. Examples include alternating pressure mattresses, foam cushions, and air-filled cushions.
6. Skin Hygiene: Keep the skin clean and dry to prevent irritation and infection. Use mild cleansers and moisturizers to maintain skin integrity. Avoid prolonged exposure to moisture, which can increase the risk of skin breakdown.
7. Regular Skin Inspections: Regularly inspecting the skin for signs of redness, discoloration, or skin breakdown is essential. Keeping the skin clean, dry, and moisturized can also help prevent irritation and breakdown.
8. Regular Exercise and Movement: Encourage regular physical activity and movement within the individual's capabilities to improve circulation and prevent muscle atrophy. Consult with a physical therapist for personalized exercise recommendations.
9. Assistive Devices and Adaptive Techniques:
Using assistive devices such as wheelchairs, cushions, and lifts can help reduce pressure on vulnerable areas. Occupational therapists can teach adaptive techniques for daily activities to minimize pressure and friction on the skin.
10. Education and Training: Individuals with SCI, caregivers, and healthcare providers should receive education and training on pressure sore prevention, early detection, and proper wound care techniques.
11. Nutrition and Hydration: Adequate nutrition and hydration are vital for maintaining skin health and promoting tissue healing. A balanced diet rich in protein, vitamins, and minerals supports skin integrity and wound healing.
12. Prompt Wound Care: If a pressure sore develops, prompt and appropriate wound care is essential to prevent infection and promote healing. This may include cleaning the wound, applying dressings, and, in some cases, surgical interventions.
13. Maintaining Overall Health: Managing underlying health conditions, such as diabetes or vascular disease, can help reduce the risk of complications associated with pressure sores.
14. Collaboration with Healthcare Team:
Individuals with SCI should work closely with their healthcare team, including physicians, nurses, physical therapists, and wound care specialists, to develop and implement a comprehensive pressure sore prevention and management plan.
Preventing pressure sores in individuals with spinal cord injury (SCI) is crucial due to the heightened risk associated with impaired sensation, limited mobility, and prolonged periods of sitting or lying down. Here are some strategies to avoid pressure sores in individuals with SCI:
By implementing these preventive measures and maintaining vigilance, individuals with SCI can reduce the risk of developing pressure sores and maintain skin integrity, leading to improved overall health and quality of life.


